“I learned a long time ago the wisest thing I can do is be on my own side, be an advocate for myself and others like me.”- Maya Angelou
We, as humans, are an odd lot. We do an excellent job of preaching to the masses about what they should do, but fail miserably at following that own advice for ourselves. I have found that human trait to be a glaring obstacle in my own life as I travel the roads with RRP and pulmonary RRP. Advocacy for you, well, it’s a thousand times easier than advocacy for myself. For myself, it can be exhausting. That leads us to todays post, “Advocacy, When It’s You.”
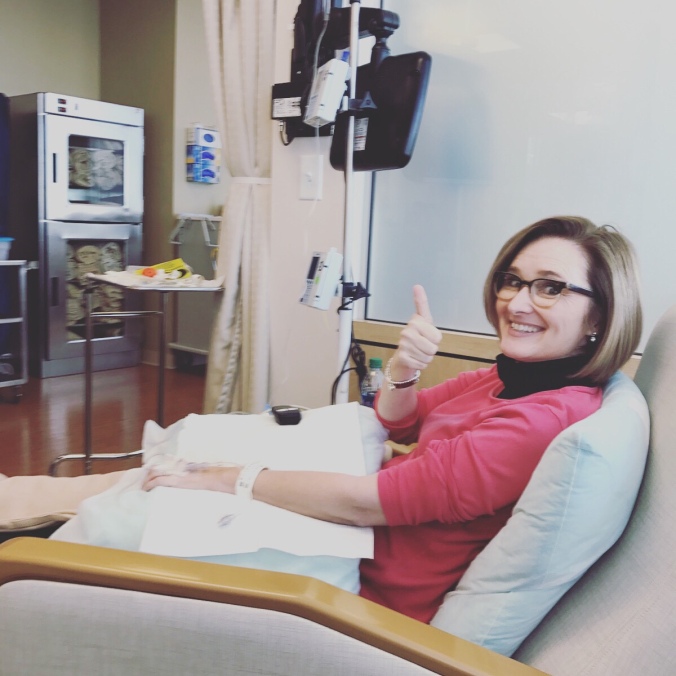
It’s been just over five years since I learned I had pulmonary metastasis of Recurrent Respiratory Papilloma. (RRP since 1972) If you believe some of the older literature on this rare complication of RRP, that would mean that I am on the flip side of the ten year stopwatch. Thankfully, because of advocacy, I know that is a misinformed expectancy based on a few cases. I know just as many far past that mark as I do that didn’t cross that ten year line. Within the past five years, I have been to the OR several times (what’s a few more on top of 250+?), had my first non-general bronchoscopy, seen the in-office snake more times that I care to recall, participated in a NIH trial using Avelumab, agreed to a power-port (my veins hate me), sat in the oncology infusion chair every three weeks for the past year (until now-update coming), inquired on a new NIH trial with the plan to go to intake in April, become a bold advocate for RRP and pulmonary RRP, and realized that as much as I wanted, and still want, to ignore this “lot in life”, I can’t. If I’m not advocating for me, then who is? If I am truly invested in the chase for the cure, I have to have the same intensity for my own disease path as I do for those I call my Warrior Family. What no one tells you is this-advocating for yourself can often feel selfish, greedy, unwarranted. We are bombarded with ads in every area of our life-ads for various diseases, cancers. Is it selfish of me to hyper focus on my disease, when there are so many diseases that need attention? It’s on those days where I ask that question that something always happens….I always get reminded that my advocacy is bigger than myself, bigger than RRP….whether it’s a new Mom of a RRP Warrior reaching out to the community for any nugget of hope that can be found, or an adult who didn’t know the disease could come back after a remission, or a person who stumbles onto a blog and learns about a disease they didn’t know existed, or a conference invitation-another opportunity to share awareness, a day where I have to tell my community of a warrior passing from conversion of the disease, the opening of a message to learn of another warrior with pulmonary disease, a day where I connect with stakeholders who could lead us to a cure, or simply share the life stories of my Warrior Family…that reminder that for my community, this disease is as big as the most heavily funded pharmaceutical on the market, it’s our world, it’s the life we live. It’s personal. It’s not just me, it’s an entire community.
So, once again, I ask you to follow my journey, in the hopes that my story helps someone, somewhere. In the hopes that my story is seen by a researcher who is focused on HPV+ solid tumors, in the hopes that a pharmaceutical sees my story and understands it’s the story of an entire Warrior Family across the world pleading for a cure. In the hopes that my story gets one family to head to their primary care and ask for the Gardasil vaccination series. In the hopes that on the days I am simply exhausted from my own disease journey, that you will use my story, our stories to help us chase the cure.
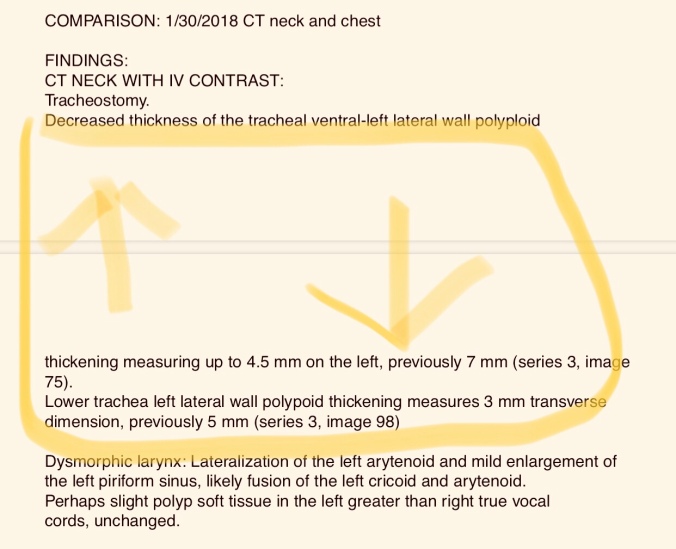
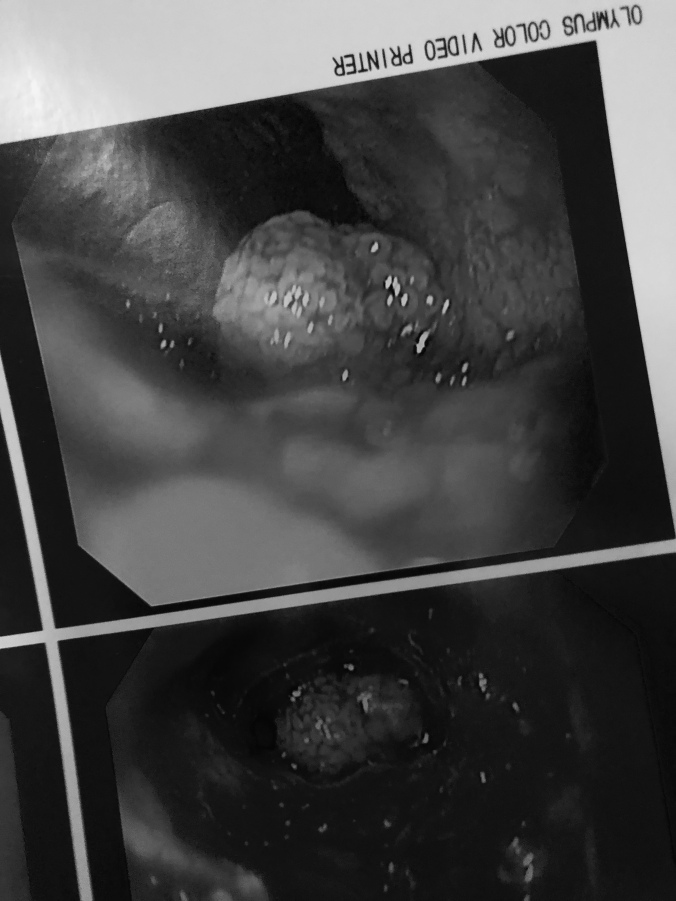
The past few months have been a roller-coaster. At some point over the summer, I developed a pain in the center of my chest. It kept increasing in intensity and frequency, and was enough to prompt cardiac exams. Nothing was found that would point to the pain, so oncology’s answer was pain meds. “It must just be a side effect.” Due to the bleeding risk of Avastin, I was put on Tramadol. From a couple times a day, to every four hours with breakthrough pain, this went on for months. Worsening cough, things coming up that resembled small aliens, countless clinic visits, and this very knowledgable advocate was in the very tailspin she works so hard to keep others out of. Thankfully, I have an advocate to lean on in these times (who I also call my friend), and she would remind me of things on the days my head simply wasn’t in the game. I never really understood how exhausting pain could be, until this issue. How powerful the pain is on your brain and your entire being. A ten week break from Avastin was requested, and I was finally able to get a bronchoscopy to view the area I knew pain was radiating from. I wish I could tell you that it was because of my care team pushing for answers, but it was because of me not giving up and trusting that I knew my body better than experts in their field. This is 2019. The pain first began summer 2018. The bronchoscopy revealed a very angry airway, with some very angry plaque at the bronchus/carina area that led up into my trachea. (Exactly where I was feeling the pain radiate from.) That was suctioned away. There was some instant pain relief, not all gone, but relief. An infection came to visit (Or was it already there and we just angered it), so it was Levaquin time. There was still pain, and still some aliens coming from my airway, so I then reached out to request an in office scope. Apx. two weeks from bronchoscopy, seven months from initial pain, we saw a tracheal ulceration. I am now on week two of another round of Levaquin, with about two more weeks of medicine left. The pain is only there when I cough, and from what was a 8 on the pain scale, it’s now a 3. Is this my new normal? Or will this resolve once ulceration is healed? Is the ulceration due to the Avastin? Did we wait too long to begin to space out infusions? If I had not kept pushing my care team, would I have developed an Avastin induced fistula? My head swirls these days thinking of the various outcomes, and the danger I could have been in. My head gets angry when I think back on all of the times I messaged, mentioned, etc.. what was happening. Angry at myself for even letting the tailspin happen. I know better, yet when it’s your care, it’s harder to follow your own advice…because that’s your apple cart you are about to flip over.
Where am I today? Today, I’m on Levaquin and the side effects can be horrible some days. I head back next week to be scoped in office to see where the ulceration is, as well as meet with a cardio-thoracic surgeon, and I will be having an endoscopy to view esophagus soon to verify no damage made its way there. We may or may not try another Avastin infusion in March, all depends on the ulceration. April should be a visit to the NIH to screen for M7824 trial. I am tired, and I wish I could wave a white flag and make it all go away, but this is my reality and I’m working to find the blessing in it so that the bad days aren’t bad weeks.
Now, how about some good news! Ya know, those blessings in the midst. I am so excited to let ya’ll know that the RRPF will be going to the World Orphan Congress in DC in April! I can hardly wait to make our presence known, and I am so thankful to Terrapin for the VIP pass. I just know we are close to finding the cure, better treatment options. How can we not be? Science is moving at warp speed these days in learning how to harness the immune system….each day we get more proof that HPV is found in far more cancers than we knew just a few years ago. Each day we get closer to global herd immunity to the HPV strains that cause cancer and RRP. We may be a community of disabled voices, but we are also a community of able voices and in our croaks and creeks, we are one voice. I know for a fact that anytime anyone with the RRPF attends a conference, we are there as an entire community-and we get stronger each day. The pulmonary arm of the RRPF is at work to find a team to help get to screening for pulmonary RRP and create a database of where patients are and who is treating them and positive outcomes-laser focused on a curative treatment. The RRPF is in the process of launching an IRB reviewed patient registry. Each day brings a little bit larger footprint.
Personal good news-I’ve been reminded how difficult being a patient is, and that will make me fight even harder for my community. So, advocacy when it’s you-yes, it hard. Yes, it will cause tears. It will mean far too many bite sized Milky-Ways go in your mouth. So, my fellow warriors, let us keep going, one foot in front of the other. A determined march to not lose another one of our community, chasing the cure with focus and determination.